Featured
Friend and Foe: How Inflammation Fights Disease and Fuels Depression
Our immune system uses inflammation to fend off infection and heal injuries, but when this system is overburdened by stress and physical illness, inflammation can also fuel mental health conditions like depression.
- Addressing inflammation as a public health issue could help improve outcomes for millions of people with depression and other mental health conditions.
- Inflammation plays an essential role in the body’s immune system not only by taking on illness and infection directly but also by changing our behavior to promote recovery.
- Stress, early adversity, and physical health conditions can throw this system out of balance, contributing to a cycle of heightened inflammation that can interfere with mental health.
- A number of proinflammatory biomarkers have been found to influence the symptoms of depression, which involve many of the same sickness behaviors commonly associated with physical illnesses.
- The specific causes and effects of inflammation differ significantly between individuals, moderated by everything from sex to socioeconomic status and cultural expectations.
- Social support and other psychosocial factors could help buffer against the effects of stress and inflammation on depression.
Inflammation today, depression tomorrow • An inflammatory start • Social causes and solutions
Symptoms like fever, fatigue, pain, and swelling are rarely welcome, but when we know our body is fighting off the flu or healing a nasty wound, these inflammatory responses can indicate that our immune system is hard at work getting us healthy again. Our immune system doesn’t only influence our physical health, however—it also influences behavior, which can in turn influence future inflammation, according to Daniel Moriarity (University of California, Los Angeles).
If a person thinks back to the last time they were sick or had a strong response to a vaccine, they probably experienced symptoms like fatigue, decreased appetite, and reduced motivation, said Moriarity in an interview with the Observer.
“These are behavioral correlates of inflammatory activity. They are historically called ‘sickness behaviors’ but, if we look at the DSM [Diagnostic and Statistical Manual of Mental Disorders], they are also symptoms of depression,” Moriarity said.
Many of the same proinflammatory proteins—known as cytokines—that the immune system releases in response to illness and injury are also produced in response to nutritionally deficient diets, reduced sleep, and stress, explained Grant S. Shields (University of California, Davis), Wesley G. Moons (Moons Analytics), and George M. Slavish (University of California, Los Angeles) in a 2017 Perspectives on Psychological Science article.
Ideally, our immune system and brain regulate one another to encourage adaptive behaviors such as lying low to conserve energy when we’re sick, the researchers wrote. The immune system produces cytokines to, among other things, influence behavior. In turn, the brain promotes or suppresses the production of cytokines in response to psychological experiences, using hormones like epinephrine, norepinephrine, and cortisol.
Sustained stress and inflammatory health conditions like diabetes, arthritis, hypertension, and obesity can cause the body’s anti-inflammatory response to become less effective, however. When stress and inflammation are chronic, the permanent state of increased inflammation can interfere with executive functioning, motivation, and perceptions of stress, discouraging behaviors like exercise, healthy eating, and socialization that could help reduce inflammation.
“From this perspective, a person’s biological milieu, psychosocial life history, thoughts, and behaviors all influence one another and interact over time to shape self-regulatory capabilities and lifespan health,” Shields and colleagues wrote.
As this connection would suggest, inflammation also appears to be a contributor to numerous mental health conditions, including anxiety and, perhaps most notoriously, depression. In 2019, an estimated 970 million people globally were living with a mental disorder, according to the World Health Organization. In the first year of the COVID-19 pandemic, the global prevalence of anxiety and depression specifically spiked 25%.
Much more research on mental health
-

Mental Health
Psychological scientists have amassed a vast amount of empirical knowledge on the causes of and best treatments for mental disorders.
-

Childhood and Adolescent Mental Health
A growing body of research connects various aspects of children’s environments and their emotional well-being.
-

Grief and Trauma
Psychological scientists are leading the way in addressing the mental health issues resulting from traumatic events.
Given that 10% to 20% of people experience depression in their lifetime, targeting inflammation as a public health issue could improve outcomes for millions of people, Alexander L. Chu (University of Texas at Austin) and colleagues wrote in a 2021 article.
“Inflammation and depression could share a similar relationship like blood pressure and stroke,” wrote Chu and colleagues. That’s not to say that inflammation is the only cause of depression, they stressed. But just as increased blood pressure reliably increases a person’s chances of suffering a stroke, increased levels of inflammation are strongly and reliably associated with an increased risk for depression.
For example, in a 2022 study of 2,761 Singaporean adults ages 55 to 98 conducted by Rong Shi (Shandong University) and colleagues, participants had more ongoing symptoms of depression if their blood had higher levels of three proinflammatory cytokines: C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNF-α). Blood levels of IL-6 and TNF-α also predicted which participants would become or still be depressed three and six years later.
“As our understanding of the complex interactions between the body, brain, and mind improves, this understanding needs to be matched with a concerted effort to develop not only new treatments but also public health strategies that recognise the broad-spectrum impact of targeting inflammation,” Chu and colleagues wrote.
Interventions that target inflammation, including anti-inflammatory medications, exercise, and stress-management programs, could be particularly valuable for people whose symptoms don’t respond to antidepressants alone, the researchers noted, as well as for people with preexisting inflammatory conditions like coronary heart disease that may increase a person’s risk of developing inflammation-related depression in the future.
Inflammation today, depression tomorrow
Until recently, most studies on inflammation and depression focused on between-person differences, allowing researchers to reach the conclusion that if one person has higher inflammation than another, they are likelier to have more symptoms of depression, Moriarity explained. Now, studies that test within-person differences in inflammation are essential to understanding the causal relationship between inflammation and depression, as well as potential pathways for treatment.
Within-person experimental studies, Moriarity noted, have suggested that artificially inducing inflammation can increase depression in participants—and, in a pair of studies published in Clinical Psychological Science in 2019 and 2020, Moriarity and colleagues sought to build on these findings by analyzing adolescent participants’ depression and inflammation levels over longer timespans.
The first of these studies, published in 2019, focused on between-person differences in inflammation and depression. The researchers collected blood samples from 201 American adolescents ages 12 to 20 years old at six points over a period of up to 31 months. When the inflammation levels in each blood sample were compared to participants’ self-reported symptoms of depression at each appointment, three specific cytokines predicted the development of symptoms: TNF-α, IL-6, and interleukin-8 (IL-8).
The effects of these cytokines differed somewhat with participants’ sex, however. While higher TNF-α levels predicted increased symptoms of depression at the next appointment for both males and females, higher IL-6 levels predicted increased depression in females, and higher IL-8 levels predicted decreased depression in males. This suggests that sex-based differences in inflammatory responses could be part of the reason why females tend to experience higher rates of depression in adolescence, Moriarity and colleagues wrote in the 2019 Clinical Psychological Science article.
The researchers’ second study of 140 adolescents, published in 2020, included within-person analyses. Participants reported their depressive symptoms and had blood drawn at up to six appointments spaced approximately 1 year apart. In this case, only TNF-α predicted depression. This could indicate that TNF-α is predictive of depression on a broader level, whereas other cytokines may be more closely related to specific symptoms or may require more time to build up in the body before influencing mental health outcomes, Moriarity and colleagues suggested.
“Naturally occurring, within-person changes are associated with changes in depression—and vice-versa—in a potentially causal positive-feedback loop,” Moriarity said of his team’s findings.
An inflammatory start
Early adversity appears to be an important risk factor for increased inflammation because of how stress encourages unhealthy behaviors, according to Elizabeth B. Raposa (University of California, Los Angeles) and colleagues in a 2014 Psychological Science article. The researchers explored this dynamic through a 2014 study of 389 mother–child pairs who had previously participated in a longitudinal birth-cohort study in Queensland, Australia.
As part of the initial study, the mothers reported on environmental factors related to their pregnancy and child-rearing experience during the first 5 years of their child’s life. Raposa and colleagues then contacted the children again at 15, 20, and 21 years old to complete a survey about their depressive symptoms, health behaviors, and stress levels and later collected one blood sample from participants when they were 22 to 25 years old.
By analyzing these data, the researchers found that adolescents raised in more adverse environments (characterized by low income, harsh discipline, and parents reporting more mental health conditions, relationship conflict, and criminal behavior) reported more symptoms of depression and chronic stress, were more likely to smoke, and had a higher body mass index (BMI) than adolescents raised in less stressful circumstances. Young adults’ smoking at age 21 predicted higher levels of tumor necrosis factor receptor type II (TNF-RII) in their blood sample, which indicates higher levels of TNF-α, and higher BMI predicted higher levels of both TNF-RII and CRP.
“Our results highlight negative health behaviors, particularly smoking and high BMI, as important pathways by which continuing life stress ‘gets under the skin’ to contribute to long-term risk for physical illness,” Raposa and colleagues wrote. “Given that maladaptive health behaviors portend inflammation in young adulthood, they serve as promising targets for interventions designed to prevent the negative consequences of early adversity.”
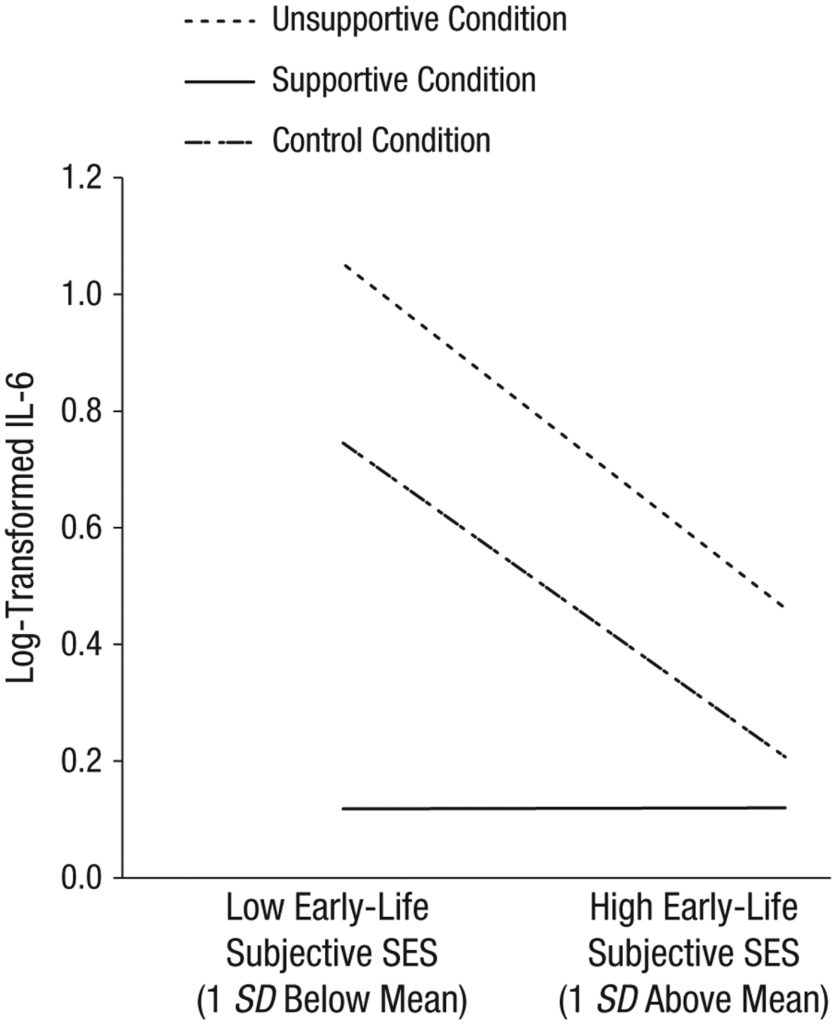
Interestingly, research suggests that although early adversity may make people uniquely susceptible to social stress, people from low-income families may also be uniquely receptive to the buffering effects of social support. In a 2015 Psychological Science study, Neha A. John-Henderson (University of Pittsburgh) and colleagues took salivary samples from 63 undergraduate students before and after they discussed a negative experience from their past with a confederate pretending to be another participant.
The IL-6 levels in the saliva of students who described themselves as having grown up in households with higher socioeconomic status (SES) remained the same regardless of how interested or disinterested the confederate pretended to be in their story.
John-Henderson, N. A., Stellar, J. E., Mendoza-Denton, R., & Francis, D. D. (2015). Socioeconomic status and social support: Social support reduces inflammatory reactivity for individuals whose early-life socioeconomic status was low. Psychological Science, 26(10), 1620–1629. https://doi.org/10.1177/0956797615595962
Students from lower SES backgrounds were far more sensitive to the confederate’s reactions. When the confederate behaved in a disinterested manner by refusing to make eye contact and sighing with boredom, the IL-6 levels of these students spiked. When the confederate behaved in a supportive manner by nodding along and making supportive comments throughout the story, however, the lower SES students’ IL-6 levels actually dropped below those of higher SES students, suggesting that they found the experience less stressful.
The effects of SES on inflammation were slightly less pronounced in John-Henderson’s second study of 97 undergraduates, but differences did emerge. Students from low- and high-SES backgrounds exhibited the same inflammatory response to a socially supportive confederate, but low-SES participants had significantly stronger IL-6 responses to the unsupportive and control conditions.
These results remained significant regardless of participants’ current SES, the researchers noted, suggesting that a person’s SES during childhood continues to influence their inflammatory responses to social stress in adulthood. People raised with access to more resources tend to think more independently, the researchers wrote, so it follows that they would be less sensitive to social support. Similarly, people raised with access to fewer resources tend to think more interdependently and are thus more likely to attend to other people’s reactions to their behavior.
“Although prior research indicates that low SES is associated with increased risk for a number of diseases, our findings suggest that the greater attunement to the interpersonal environment also associated with low SES could serve as an important protective factor,” John-Henderson and colleagues wrote.
The exact relationship between social behavior and inflammation may differ across cultures. In a 2015 Psychological Science article, for example, APS Fellow and Past-President Shinobu Kitayama (University of Michigan) and colleagues compared how negative emotions influenced the health risk factors, including inflammation, of 1,045 American and 382 Japanese adults. Drawing on surveys about how each participant expressed and suppressed feelings of anger, Kitayama and colleagues found that Americans who expressed more anger had more health risks—including increased levels of IL-6 and CRP in addition to higher blood pressure and cholesterol—than their more serene peers. This is consistent with the prevailing notion that anger is bad for your cardiovascular health, Kitayama explained to the Observer.
By contrast, Japanese participants who expressed anger more frequently had fewer health risk factors than those who did so less often. This could be because of differences in when anger is expressed across cultures, Kitayama and colleagues suggested. In more individualist Western cultures like that in the United States, people with lower status, who generally have worse health outcomes, may be more likely to express anger in response to not being able to achieve their goals, the researchers explained. In more interdependent cultures like that in Japan, on the other hand, anger is perceived as more socially disruptive and undesirable, meaning that only those with high social status, who have better health outcomes, can afford to express it.
“This novel finding casts doubt on the currently dominant assumption that anger expression and hostility have adverse effects on health,” Kitayama and colleagues concluded. “It thus highlights the importance of incorporating cultural perspectives into the analysis of anger expression, and especially its effects on physical health.”
Social causes and solutions
The social-signal-transduction theory of depression provides one explanation for how social stress contributes to a cycle of inflammation and increased risk of depression, Annelise A. Madison (The Ohio State University) said in an interview with the Observer.
“Social stress, especially conflict and exclusion-related stress, provokes an immune response, perhaps because the body is preparing for the possibility of attack or wounding, which is more common if an individual is separated from their group,” Madison said. “In the context of frequent and repetitive social stress, people may never fully recover, and inflammation may not return to baseline and instead remain elevated.”
Maintaining elevated levels of inflammation consumes a lot of metabolic resources, Madison continued, resulting in a number of symptoms of depression intended to help conserve energy, including anhedonia, hypersomnia, and low mood.
This dynamic was evident in a pair of 2021 Psychological Science studies Madison and colleagues conducted with 38 married couples and a group of 79 breast cancer survivors. In both cases, participants reported their symptoms of depression and stress levels and had their blood drawn before completing a stressful social task. For the couples, the task entailed discussing an ongoing problem in their relationship; the breast cancer survivors were required to give a speech. The researchers then took two additional blood samples from each participant over the next several hours.
When the married couples returned for their second appointment, participants who reported experiencing more interpersonal stress in their daily lives and had a greater increase in IL-6 in response to the social-stress task during their first visit were more likely to report increased symptoms of depression at their second visit. Similarly, all breast cancer survivors who reported receiving less social support in their daily lives during their first visit reported an increase in depression at their second appointment. This was particularly pronounced among participants whose TNF-α levels increased more during the social-stress task.
“Our findings suggest that exaggerated inflammatory reactivity is not only a correlate of but also a risk factor for heightened depressive symptoms, especially in the context of chronic or frequent interpersonal stress,” Madison and colleagues wrote. “Current evidence suggests that inflammation and depression fuel one another—a vicious cycle.”
Increased inflammation doesn’t make depression inevitable, though. In a 2022 Psychological Science study of 187 people with early-stage breast cancer, Andrew W. Manigault (University of California, Los Angeles) and colleagues found that participants with higher levels of CRP were more likely to become depressed over the 18-month study period. However, this was only true when they reported high levels of cancer-related stress and few psychosocial resources (such as close social relationships, optimism, high self-esteem, mindfulness, and a sense of control over their lives) with which to combat it. When participants reported having more psychosocial resources to draw on, increased stress was less likely to increase their symptoms of depression, and the effects of inflammation on depression were also reduced.
These and other psychosocial sources of resilience could help explain why many people do not become depressed in response to deeply stressful events. They could also provide a path forward for people who do, Manigault and colleagues wrote. Inflammation and stress do appear to fuel a range of mental and physical maladies, but research on the mind–body connection suggests that the cycle can be broken.
Feedback on this article? Email [email protected] or login to comment. Interested in writing for us? Read our contributor guidelines.
Chu, A. L., Hickman, M., Steel, N., Jones, P. B., Davey Smith, G., & Khandaker, G. M. (2021, July). Inflammation and depression: A public health perspective. Brain, Behavior, and Immunity, 95, 1–3. https://doi.org/10.1016/j.bbi.2021.04.015
John-Henderson, N. A., Stellar, J. E., Mendoza-Denton, R., & Francis, D. D. (2015). Socioeconomic status and social support: Social support reduces inflammatory reactivity for individuals whose early-life socioeconomic status was low. Psychological Science, 26(10), 1620–1629. https://doi.org/10.1177/0956797615595962
Kitayama, S., Park, J., Boylan, J. M., Miyamoto, Y., Levine, C. S., Markus, H. R., Karasawa, M., Coe, C. L., Kawakami, N., Love, G. D., & Ryff, C. D. (2015). Expression of anger and ill health in two cultures: An examination of inflammation and cardiovascular risk. Psychological Science, 26(2), 211–220. https://doi.org/10.1177/0956797614561268
Madison, A. A., Andridge, R., Shrout, M. R., Renna, M. E., Bennett, J. M., Jaremka, L. M., Fagundes, C. P., Belury, M. A., Malarkey, W. B., & Kiecolt-Glaser, J. K. (2021). Frequent interpersonal stress and inflammatory reactivity predict depressive-symptom increases: Two tests of the social-signal-transduction theory of depression. Psychological Science, 33(1), 152–164. https://doi.org/10.1177/09567976211031225
Manigault, A. W., Kuhlman, K. R., Irwin, M. R., Cole, S. W., Ganz, P. A., Crespi, C. M., & Bower, J. E. (2022). Psychosocial resilience to inflammation-associated depression: A prospective study of breast-cancer survivors. Psychological Science, 33(8), 1328–1339. https://doi.org/10.1177/09567976221079633
Moriarity, D. P., Kautz, M. M., Mac Giollabhui, N., Klugman, J., Coe, C. L., Ellman, L. M., Abramson, L. Y., & Alloy, L. B. (2020). Bidirectional associations between inflammatory biomarkers and depressive symptoms in adolescents: Potential causal relationships. Clinical Psychological Science, 8(4), 690–703. https://doi.org/10.1177/2167702620917458
Moriarity, D. P., Mac Giollabhui, N., Ellman, L. M., Klugman, J., Coe, C. L., Abramson, L. Y., & Alloy, L. B. (2019). Inflammatory proteins predict change in depressive symptoms in male and female adolescents. Clinical Psychological Science, 7(4), 754–767. https://doi.org/10.1177/2167702619826586
Raposa, E. B., Bower, J. E., Hammen, C. L., Najman, J. M., & Brennan, P. A. (2014). A developmental pathway from early life stress to inflammation: The role of negative health behaviors. Psychological Science, 25(6), 1268–1274. https://doi.org/10.1177/0956797614530570
Shi, R., Gwee, X., Chua, D. Q. L., Tan, C. T. Y., Yap, K. B., Larbi, A., Lu, Y., & Ng, T. P. (2022, August) Inflammatory markers and incident depression: Evidence in a population-based prospective study. Psychoneuroendocrinology, 142, Article 105806. https://doi.org/10.1016/j.psyneuen.2022.105806
Shields, G. S., Moons, W. G., & Slavich, G. M. (2017). Inflammation, self-regulation, and health: An immunologic model of self-regulatory failure. Perspectives on Psychological Science, 12(4), 588–612. https://doi.org/10.1177/1745691616689091






APS regularly opens certain online articles for discussion on our website. Effective February 2021, you must be a logged-in APS member to post comments. By posting a comment, you agree to our Community Guidelines and the display of your profile information, including your name and affiliation. Any opinions, findings, conclusions, or recommendations present in article comments are those of the writers and do not necessarily reflect the views of APS or the article’s author. For more information, please see our Community Guidelines.
Please login with your APS account to comment.