Measuring Pain With a Flash
 In the doctor’s office, patients often are asked to rate their symptoms of pain on a continuous scale typically ranging from 1 (least painful) to 10 (most painful). This type of scale is called a visual analog scale (VAS). But if two patients rate their pain a 7 out of 10, there’s no guarantee that those numbers mean the same thing. A 7 from an individual with fibromyalgia, a painful medical condition, is probably much more intense in an absolute sense than a 7 from a healthy young child who has just scraped a knee.
In the doctor’s office, patients often are asked to rate their symptoms of pain on a continuous scale typically ranging from 1 (least painful) to 10 (most painful). This type of scale is called a visual analog scale (VAS). But if two patients rate their pain a 7 out of 10, there’s no guarantee that those numbers mean the same thing. A 7 from an individual with fibromyalgia, a painful medical condition, is probably much more intense in an absolute sense than a 7 from a healthy young child who has just scraped a knee.
APS Past President Linda M. Bartoshuk (University of Florida) and her colleagues have applied a technique called magnitude matching to measure the intensity of experiences, including pain, more accurately. Using this technique, researchers ask individuals to compare the intensity of one stimulus to the intensity of another that is unrelated. To illustrate, imagine that you shine a bright light and then ask individuals to rate the intensity of their pain relative to the intensity of the light. Now, differences emerge: The fibromyalgia patient in great pain, for example, might maintain his or her pain rating of 7, whereas the child might provide a rating of 3 — the bright light is intense, whereas the pain of the skinned knee is less intense by comparison.
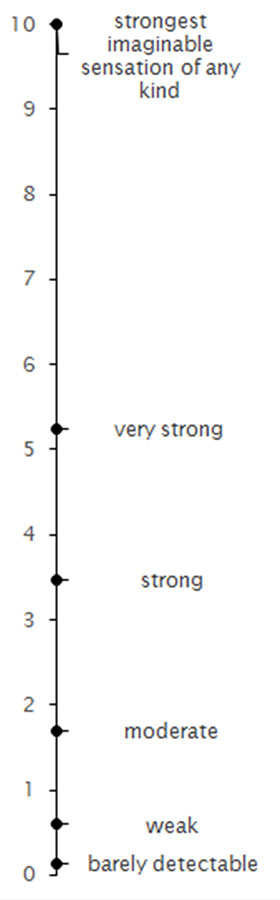
In related work, Bartoshuk and colleagues have explored the effectiveness of different scales at rating subjective experiences. They have determined that a scale ranging from barely detectable to strongest imaginable sensation of any kind well captures the ways in which stimuli differ in intensity. This scale is called the general Labeled Magnitude Scale (gLMS; see figure), and other researchers have found that it is effective for measuring pain.
The VAS is complicated by ceiling effects — patients might enter a hospital rating their pain as a 10, for example, but don’t have space to increase their rating if the pain becomes more intense. In one study, Marlís González-Fernández (Johns Hopkins University) and her colleagues had 80 pain-clinic patients rate their pain using both the VAS and the gLMS. The researchers found that patients rated their pain on the VAS as 6.13 out of 10, on average, whereas the same patients rated their pain on the gLMS as 4.35 out of 10.
The authors concluded that using the gLMS had the benefit of “reducing the ceiling effect and allowing for rating worsening pain at the higher end of the scale.” And administering the gLMS took minimal time for clinicians, only requiring about 2.5 minutes.
The measurement of pain has important implications, Bartoshuk says.
“When investigators do not use modern methods, they run the risk of missing differences between groups that are real,” she says. “As our scaling gets better, we are likely to come to some fascinating insights about differences among us.”
References and Further Reading
Bartoshuk, L. M., Duffy, V. B., Chapo, A. K., Fast, K., Yiee, J. H., Hoffman, H. J., … Snyder, D. J. (2004). From psychophysics to the clinic: Missteps and advances. Food Quality and Preference, 15, 617–632. doi:10.1016/j.foodqual.2004.05.007
Bartoshuk, L. M., Fast, K., & Snyder, D. J. (2005). Differences in our sensory worlds: Invalid comparisons with labeled scales. Current Directions in Psychological Science, 14, 122–125. doi:10.1111/j.0963-7214.2005.00346.x
González-Fernández, M., Ghosh, N., Ellison, T., McLeod, J. C., Pelletier, C. A., & Williams, K. (2014). Moving beyond the limitations of the visual analog scale for measuring pain: Novel use of the general labeled magnitude scale in a clinical setting. American Journal of Physical Medicine & Rehabilitation, 93, 75–81. doi:10.1097/PHM.0b013e31829e76f7





Comments
With such a large spread between strong and super-strong pain, i wondered about the reliability of self-reports, e.g., in a case where the pain is expected to be consistent, does the actual rating of pain vary when reported at different times or is it also pretty stable?
APS regularly opens certain online articles for discussion on our website. Effective February 2021, you must be a logged-in APS member to post comments. By posting a comment, you agree to our Community Guidelines and the display of your profile information, including your name and affiliation. Any opinions, findings, conclusions, or recommendations present in article comments are those of the writers and do not necessarily reflect the views of APS or the article’s author. For more information, please see our Community Guidelines.
Please login with your APS account to comment.